AmeriSys resolves work comp claims faster with Head Injury and COVID Management programs

Last week we discussed two 2022 workers’ compensation care upgrades, Rebound and RapidResponse, that not only significantly help resolve claims more quickly, but also lower payouts and reduce litigation costs for employers and insurers. Even more important, they provide injured employees the latest in quality medical care and returning them to gainful employment. Today we’ll discuss two more initiatives, our Head Injury program and our BADGE program that now includes COVID-19 disease management. All four programs will help us resolve work comp claims faster, saving our employers and insurers time and money. View last week's post here.
Head Injury Program
Our Head Injury Program is both a URAC initiative and an advocacy component of our existing programs. URAC brought this initiative to the forefront with the recent recognition of the significance of even minor head injuries. Everest, our carrier partner on this initiative, had several claims from minor and untreated hits to the head that took place two or three years ago, and now have caused major injury issues. Examples are football players, from kids to pros, who’ve experienced multiple minor concussions. This program focuses on these supposedly minor injuries that later are causing post-concussion syndrome headaches, memory loss and more.
In this program, whenever a head injury is diagnosed, a nurse case manager escalates immediate care. This includes ensuring proper evaluations and individualized treatment, improving/enhancing return-to-work outcomes, reducing disability duration, resolving work comp claims faster and promoting a holistic approach to each patient’s individualized rehabilitation plan. In other words, it focuses on early identification to ensure that the proper assessments and evaluations are being completed.
Head injury case study
In October, the employee was sitting in his car while parked on the street. Someone opened his door and hit him with a baseball bat. He was diagnosed with post-concessional syndrome, depression, anxiety, sleep disorder, neck injury, right ear injury, right forearm injury, left forearm injury . Using proactive case management intervention tailored for the individual, the worker was released to full duty four months later and successfully returned to work.
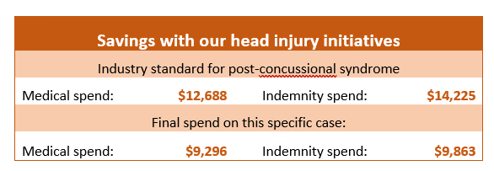
Here’s the savings, thanks to our head injury program:
Our head injury initiative saved the employer’s insurance company more than $7,700.
The BADGE program now includes COVID-19 disease management
The BADGE program, established to manage presumption issues for First Responders, now includes COVID-19 disease management. First responders who have contracted COVID-19 in the course of their employment and are experiencing long term effects need treatment by cardiologists, pulmonologists and neurologists. This program assists these patients in obtaining the care they need for this challenging condition.
Additional medical initiatives for 2022
In addition to the four programs discussed in this and our last blogpost, we’re also deploying the following tools:
- Whole Person Assessment, a disability assessment tool that can be used for funding a claim where there is anticipated permanent impairment.
- Non-Certified Surgery Program begins when surgery is denied and evaluates Peer Review denial reason, facilitates an appeal if appropriate, and conferences with treaters for a treatment plan.
- Pre-Surgical Pain Screening Program begins after surgery is approved. It includes a pre-surgical assessment and patient sessions prior to and after surgery, to support recovery.
- Enhanced Pharmacy Program, in partnership with Optum, that focuses on the safety, efficacy and cost containment of pharmaceuticals.
- Medical Clearance focuses on minimizing treatment delays. Medical clearance often accompanies requests for surgical interventions. When we see treatment delays because medical clearance is determined to be not medically necessary, we can intervene and, if necessary, work to overrule that decision.
- Functional Rehabilitation Program (FRP). While these programs can be costly, they also can help with chronic pain management. We scrutinize any FRP requests to ensure they’re approved on appropriate claims and work with medical providers to create tailored alternative treatment plans.
This blogpost originally appeared on American Claims Management's blog. The programs outlined here are a collaboration between sister companies ACM, PGCS, AmeriSys and USIS.
